We have a number of ways to pay your bills online quickly and securely. Click the appropriate button below to pay your bill. Payments can be made by check, debit or credit card.
Using the Customer Service functions you also can contact us about questions or problems with your account(s) and submit changes to your street address or insurance information.
St. Josephs/Candler is committed to extending financial assistance to qualifying patients. If payment could create a financial hardship for you, our staff will work with you to apply for assistance. Go here to read more or call Customer Service at 912-819-8455 or 800-374-7054.
You have the right to receive a “Good Faith Estimate” explaining how much your medical care will cost. Under the law, health care providers need to give patients who dont have insurance or who are not using insurance an estimate of the bill for medical items and services.
For questions or more information about your right to a Good Faith Estimate, visit www.cms.gov/nosurprises or call 1-800-985-3059.
When you get emergency care or get treated by an out-of-network provider at an in-network hospital or ambulatory surgical center, you are protected from surprise billing or balance billing.
When you see a doctor or other health care provider, you may owe certain out-of-pocket costs, such as a copayment, coinsurance, and/or a deductible. You may have other costs or have to pay the entire bill if you see a provider or visit a health care facility that isn’t in your health plan’s network.
“Out-of-network” describes providers and facilities that haven’t signed a contract with your health plan. Out-of-network providers may be permitted to bill you for the difference between what your plan agreed to pay and the full amount charged for a service. This is called “balance billing.” This amount is likely more than in-network costs for the same service and might not count toward your annual out-of-pocket limit.
“Surprise billing” is an unexpected balance bill. This can happen when you can’t control who is involved in your care—like when you have an emergency or when you schedule a visit at an in- network facility but are unexpectedly treated by an out-of-network provider.
If you have an emergency medical condition and get emergency services from an out-of- network provider or facility, the most the provider or facility may bill you is your plan’s in- network cost-sharing amount (such as copayments and coinsurance). You can’t be balance billed for these emergency services. This includes services you may get after you’re in stable condition unless you give written consent and give up your protections not to be balanced billed for these post-stabilization services.
The state of Georgia and the federal government both have laws to protect you from balance billing although they are a little different. State rules only apply to fully insured commercial health insurance plans and some government plans. Federal rules may also apply to commercial health insurance in situations where you received health care services in another state, your health insurance is regulated by a state other than Georgia or the health care service you received is not regulated by the state law. Most of the differences between the state and federal laws are in the way the rules affect providers and health insurers, so you usually won’t need to worry about that. However, the grievance processes are different, as indicated on the government websites linked below.
When you get services from an in-network hospital or ambulatory surgical center, certain providers there may be out-of-network. In these cases, the most those providers may bill you is your plan’s in-network cost-sharing amount. This applies to emergency medicine, anesthesia, pathology, radiology, laboratory, neonatology, assistant surgeon, hospitalist, or intensivist services. These providers can’t balance bill you and may not ask you to give up your protections not to be balance billed. Under Georgia law this rule also applies to imaging centers, birthing centers, and similar facilities in addition to hospitals and ambulatory surgical centers. If you get other services at these in-network facilities, out-of-network providers can’t balance bill you, unless you give written consent and give up your protections.
You’re never required to give up your protections from balance billing. You also aren’t required to get care out-of-network. You can choose a provider or facility in your plan’s network.
The best way to find an in-network provider is to use the online provider directory on your health plan’s website.
If you believe you’ve been wrongly billed, first contact your provider and/or your health plan for an explanation. If they can’t resolve your concerns, you can contact the Georgia Office of the Commissioner of Insurance and Safety Fire online at https://oci.georgia.gov/ or by phone at (404) 656-2070.
We also offer extended payment plans to patients through our partner, MedFinancial. They offer no-interest payment plans that are tailored to your health and financial situation. They are not a traditional credit card nor are they a collection agency. Their program covers all patients regardless of balance or credit history – and they never report to credit bureaus. Their customized payment options offer many benefits including:
Our team will work with you to determine the right plan for your situation, helping you pay in regular low-monthly installments you can realistically manage. To learn more, speak to one of our representatives by call 912-819-8455.
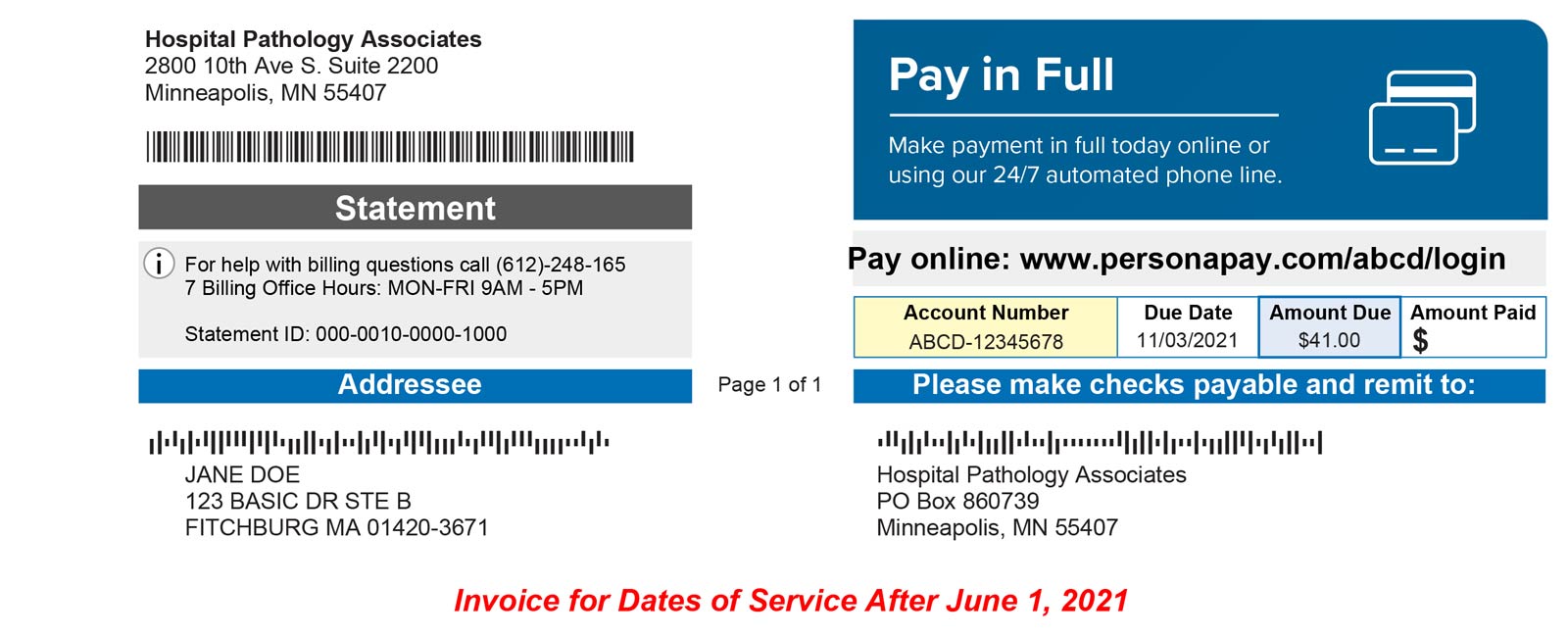
Paying your medical bills can be confusing, especially when multiple providers are involved If you had lab testing done through Chatham Pathology Associates, here is what you need to know about paying that bill conveniently online
Who is Chatham Pathology Associates?
Chatham Pathology Associates (CPA) is a pathology lab that provides testing services for patients at St. Joseph’s/Candler and other medical facilities in Savannah, Georgia. When your doctor orders lab tests like blood work or pathology samples, CPA performs the actual lab analysis.
As the testing facility CPA will bill you separately from the hospital or doctor’s office visit fee. It is common to get a bill from the lab in addition to your physician’s bill after a medical appointment when lab tests were performed.
Why You Get a Separate Bill from the Lab
Labs like CPA bill patients directly because they are usually independent companies, not owned by the hospital or doctor’s office. The lab performed services for you and needs to be paid for their work.
That’s why you will get a bill from CPA after they analyze your lab tests, in addition to any provider bills. It may come from CPA directly or go through a billing service that handles their invoices. Either way, you are responsible for paying the lab fee.
How to Pay Your CPA Bill
You have a few convenient options to pay your bill from Chatham Pathology Associates:
Pay Online
The easiest way to pay your CPA bill is through their online patient portal. You can pay by credit card or debit card online without mailing anything.
To pay online, first make sure you have received a statement with your account number. Then visit the website myaccount.apsmedbill.com and either create an account or log in if you already have one.
Select Chatham Pathology Associates from the list of providers. Enter your account number and date of birth. Then you can view your bill and make a payment by card.
Pay by Phone
If you prefer to pay over the phone, call APS Medical Billing at (419) 866-1804. Let them know you want to make a payment on your Chatham Pathology Associates account.
You will need to provide your account number from the statement. Have your credit or debit card ready to make the payment.
Mail a Check
Paying by check is another option. Make your check payable to Chatham Pathology Associates. Write your account number on the check if possible.
Mail your check to:
Chatham Pathology Associates
PO Box 638957
Cincinnati, OH 45263-8957
Be sure to allow enough time for your check to arrive before the due date. Mailed payments can take 7-10 days to process.
Use Bill Pay Through Your Bank
If your bank offers online bill pay services, you can use that to pay your CPA invoice. Just set up the payment through your bank’s website.
Provide the Chatham Pathology Associates address above and your account number. Schedule the payment to arrive by the due date.
Bill pay through your bank account can take around 5 business days. Make sure to allow enough processing time.
What to Do if You Can’t Pay the Full Amount
If paying the full lab bill is a hardship, don’t panic. You may qualify for financial assistance or a payment plan.
Chatham Pathology Associates offers options for patients who can’t afford their bill, including:
- Reduced-cost care based on your income
- Extended payment plans
- Interest-free loans to pay medical bills
To find out what options are available for your situation, call the CPA business office at (912) 819-6370. Let them know you need help with payment.
They can check if you qualify for any financial assistance programs that lower or eliminate your bill. They can also set up manageable monthly payments if needed.
Don’t ignore bills from Chatham Pathology Associates. Call them if you are having trouble paying so you can work out an appropriate solution and keep your accounts in good standing.
Other Billing Questions?
If you have any other questions about your Chatham Pathology Associates bill, you can:
-
Call the CPA business office at (912) 819-6370
-
Email questions to [email protected]
-
Mail written inquiries to:
Chatham Pathology Associates
Attn: Business Office
5353 Reynolds St.
Savannah, GA 31405
The billing staff can look up your account, explain the charges, provide copies of statements, and help with any payment issues.
Getting a separate bill from the lab can be confusing at first. But Chatham Pathology Associates offers convenient online and phone payment options to easily take care of your lab invoice. Just be sure to pay the bill or make arrangements if you need assistance. Doing so will keep your credit in good standing and your access to needed lab services in the future.
St. Joseph’s Hospital Campus 11705 Mercy Blvd. Savannah, GA 31419
We have a number of ways to pay your bills online quickly and securely. Click the appropriate button below to pay your bill. Payments can be made by check, debit or credit card.
Using the Customer Service functions you also can contact us about questions or problems with your account(s) and submit changes to your street address or insurance information.
St. Josephs/Candler is committed to extending financial assistance to qualifying patients. If payment could create a financial hardship for you, our staff will work with you to apply for assistance. Go here to read more or call Customer Service at 912-819-8455 or 800-374-7054.
You have the right to receive a “Good Faith Estimate” explaining how much your medical care will cost. Under the law, health care providers need to give patients who dont have insurance or who are not using insurance an estimate of the bill for medical items and services.
- You have the right to receive a Good Faith Estimate for the total expected cost of any non-emergency items or services. This includes related costs like medical tests, prescription drugs, equipment and hospital fees.
- Make sure your health care provider gives you a Good Faith Estimate in writing at least one business day before your medical service or item. You can also ask your health care provider, and any other provider you choose, for a Good Faith Estimate before you schedule an item or service.
- If you receive a bill that is at least $400 more than your Good Faith Estimate, you can dispute the bill.
- Make sure to save a copy or picture of your Good Faith Estimate.
For questions or more information about your right to a Good Faith Estimate, visit www.cms.gov/nosurprises or call 1-800-985-3059.
Your Rights and Protections Against Surprise Medical Bills
When you get emergency care or get treated by an out-of-network provider at an in-network hospital or ambulatory surgical center, you are protected from surprise billing or balance billing.
What is “balance billing” (sometimes called “surprise billing”)?
When you see a doctor or other health care provider, you may owe certain out-of-pocket costs, such as a copayment, coinsurance, and/or a deductible. You may have other costs or have to pay the entire bill if you see a provider or visit a health care facility that isn’t in your health plan’s network.
“Out-of-network” describes providers and facilities that haven’t signed a contract with your health plan. Out-of-network providers may be permitted to bill you for the difference between what your plan agreed to pay and the full amount charged for a service. This is called “balance billing.” This amount is likely more than in-network costs for the same service and might not count toward your annual out-of-pocket limit.
“Surprise billing” is an unexpected balance bill. This can happen when you can’t control who is involved in your care—like when you have an emergency or when you schedule a visit at an in- network facility but are unexpectedly treated by an out-of-network provider.
You are protected from balance billing for:
Emergency services
If you have an emergency medical condition and get emergency services from an out-of- network provider or facility, the most the provider or facility may bill you is your plan’s in- network cost-sharing amount (such as copayments and coinsurance). You can’t be balance billed for these emergency services. This includes services you may get after you’re in stable condition unless you give written consent and give up your protections not to be balanced billed for these post-stabilization services.
The state of Georgia and the federal government both have laws to protect you from balance billing although they are a little different. State rules only apply to fully insured commercial health insurance plans and some government plans. Federal rules may also apply to commercial health insurance in situations where you received health care services in another state, your health insurance is regulated by a state other than Georgia or the health care service you received is not regulated by the state law. Most of the differences between the state and federal laws are in the way the rules affect providers and health insurers, so you usually won’t need to worry about that. However, the grievance processes are different, as indicated on the government websites linked below.
Certain services at an in-network hospital, ambulatory surgical center or other facility
When you get services from an in-network hospital or ambulatory surgical center, certain providers there may be out-of-network. In these cases, the most those providers may bill you is your plan’s in-network cost-sharing amount. This applies to emergency medicine, anesthesia, pathology, radiology, laboratory, neonatology, assistant surgeon, hospitalist, or intensivist services. These providers can’t balance bill you and may not ask you to give up your protections not to be balance billed. Under Georgia law this rule also applies to imaging centers, birthing centers, and similar facilities in addition to hospitals and ambulatory surgical centers. If you get other services at these in-network facilities, out-of-network providers can’t balance bill you, unless you give written consent and give up your protections.
You’re never required to give up your protections from balance billing. You also aren’t required to get care out-of-network. You can choose a provider or facility in your plan’s network.
The best way to find an in-network provider is to use the online provider directory on your health plan’s website.
When balance billing isn’t allowed, you also have the following protections:
- You are only responsible for paying your share of the cost (like the copayments, coinsurance, and deductibles that you would pay if the provider or facility was in-network). Your health plan will pay out-of-network providers and facilities directly.
- Your health plan generally must:
- Cover emergency services without requiring you to get approval for services in advance (prior authorization). Under Georgia law, your health plan cannot later deny such services because they don’t consider them medically necessary.
- Cover emergency services by out-of-network providers.
- Base what you owe the provider or facility (cost-sharing) on what it would pay an in-network provider or facility and show that amount in your explanation of benefits.
- Count any amount you pay for emergency services or out-of-network services toward your deductible and out-of-pocket limit.
If you believe you’ve been wrongly billed, first contact your provider and/or your health plan for an explanation. If they can’t resolve your concerns, you can contact the Georgia Office of the Commissioner of Insurance and Safety Fire online at https://oci.georgia.gov/ or by phone at (404) 656-2070.
Visit https://www.cms.gov/nosurprises for more information about your rights under federal law.
Visit https://oci.georgia.gov/how-do-i-file-complaint for more information about your rights under Georgia law.
We also offer extended payment plans to patients through our partner, MedFinancial. They offer no-interest payment plans that are tailored to your health and financial situation. They are not a traditional credit card nor are they a collection agency. Their program covers all patients regardless of balance or credit history – and they never report to credit bureaus. Their customized payment options offer many benefits including:
- No credit reporting
- Everyone is accepted
- No hidden fees
- Easy payment methods: online, phone, check, auto pay
- Combined statements that include other medical bills and family members
Our team will work with you to determine the right plan for your situation, helping you pay in regular low-monthly installments you can realistically manage. To learn more, speak to one of our representatives by call 912-819-8455.